Hospice Eligibility Guidelines
By Joseph Shega, MD, Chief Medical Officer, VITAS Healthcare
Timely and appropriate identification of hospice-eligible patients increases the likelihood that they and their families will benefit from compassionate, end-of-life care. By law, healthcare professionals must certify that patients meet guidelines to be eligible for a referral to a hospice provider.
Table of Contents
- Who Is Eligible for Hospice Care?
- Hospice Eligibility FAQs
- Disease-Specific Guidelines for Hospice Eligibility
Who Is Eligible for Hospice Care?
For a patient to be eligible for hospice, consider the following guidelines:
- The illness is terminal (a prognosis of ≤ 6 months) and the patient and/or family has elected palliative care.
- The patient has a declining functional status as determined by either:
- Palliative Performance Scale (PPS) rating of ≤ 50%-60%
- Dependence in 3 of 6 Activities of Daily Living (ADLs)
- The patient has alteration in nutritional status, e.g., > 10% loss of body weight over last 4-6 months
- The patient has an observable and documented deterioration in overall clinical condition in the past 4-6 months, as manifested by at least one of the following:
- ≥ 3 hospitalizations or ED visits
- Decrease in tolerance to physical activity
- Decrease in cognitive ability
- Other comorbid conditions
These guidelines—provided as a convenient tool and not as a replacement for a physician’s professional judgment—help physicians determine when their patients meet clinical guidelines for hospice eligibility for life-limiting illnesses.
Free Download: Hospice Eligibility Checklist
Hospice Eligibility FAQs
Below are some common questions about hospice eligibility. Clinicians seeking additional information should consult the disease-specific pages below, explore the benefits of hospice and palliative care, or contact VITAS to discuss hospice and your practice.
How long must a patient typically have to live to qualify for hospice care?
A patient becomes eligible for hospice when their attending physician and a hospice doctor—either the hospice’s medical director or the director’s designee—agree the patient has a life expectancy of six months or less if their disease runs its normal course.
No prediction is certain, and a patient may live longer than six months in hospice. In these cases, the patient can continue receiving hospice care as long as their six-month prognosis is recertified by their hospice physician every 60 days thereafter.
What diagnosis is not allowed for hospice?
Clinicians refer patients to hospice based on a specific underlying disease state that is contributing to a prognosis of six months or less. The hospice physician may collaborate with the referring or attending physician to determine which diagnosis is most contributing to the terminality of the patient, but ultimately it is the decision of the hospice team.
Non-specific conditions or symptoms cannot be listed as the primary hospice diagnosis. For example, debility and failure to thrive may contribute to the terminal decline of a patient, but the underlying condition—such as heart failure or chronic obstructive pulmonary disease (COPD)—would be the primary hospice diagnosis.
The National Hospice and Palliative Care Organization provides a full list of ICD-9 and ICD-10 codes that cannot be used as primary diagnoses when referring patients to hospice.
Disease-Specific Guidelines for Hospice Eligibility
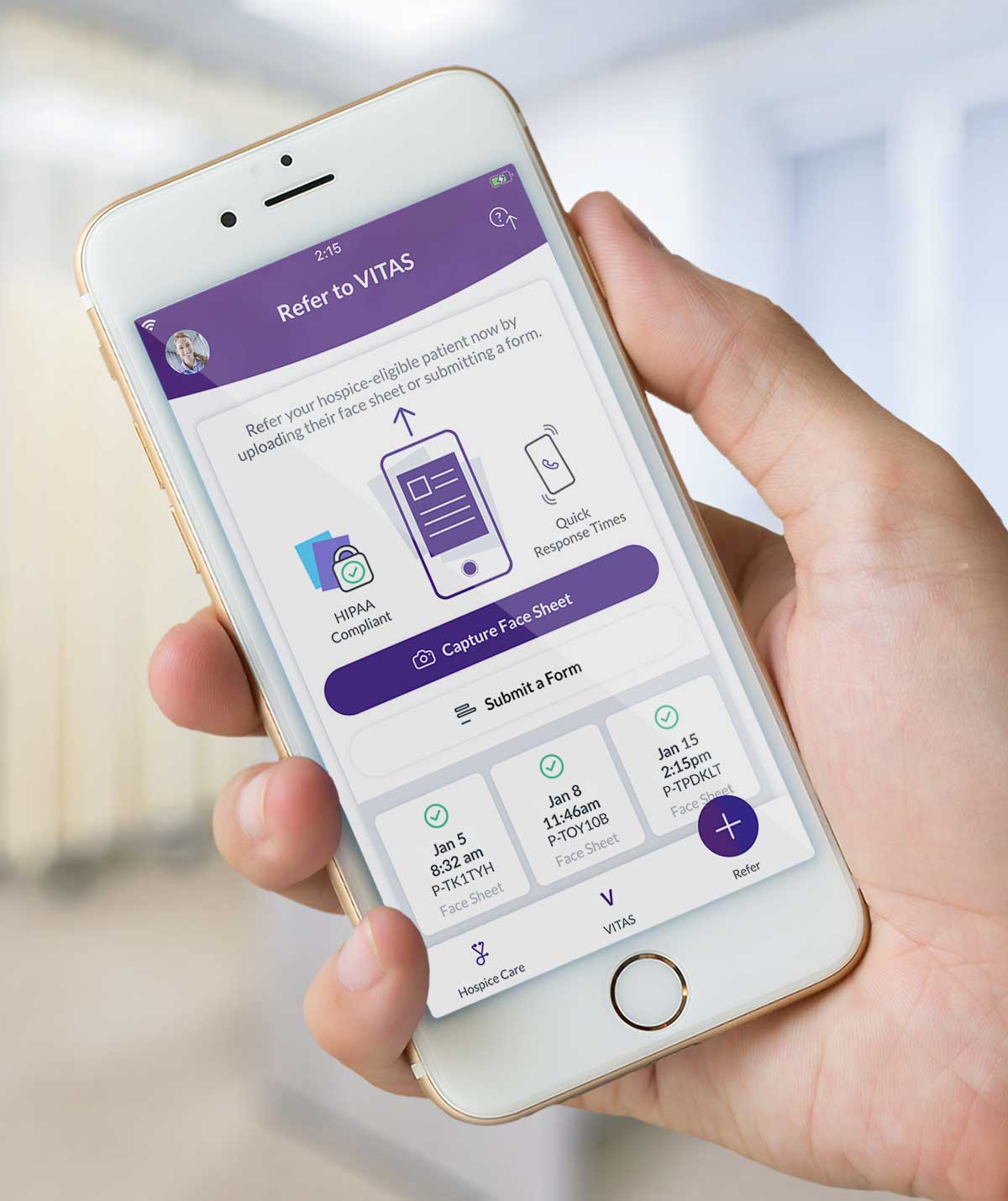
Ready for Referral?
Refer your hospice-eligible patient easily. The VITAS app features:
- HIPAA-compliant hospice referrals
- Interactive scale to determine eligibility
- Disease-specific guidelines
Available for Android and iOS devices.
Download now